EECP Therapy: Research Driven Innovation in Cardiovascular Care
Cardiovascular disease (CVD) remains the leading cause of death worldwide, accounting for nearly 18 million deaths annually, according to the World Health Organization. In this context, alternative and non-invasive therapies such as Enhanced External Counter-pulsation (EECP) have emerged as promising tools to improve patient outcomes—particularly for those with chronic angina, heart failure, and poor peripheral circulation. While EECP has been approved in several countries, including the United States, its adoption is still growing globally. This blog aims to explore EECP from multiple dimensions: its clinical science, global research footprint, credibility in evidence-based medicine, and its potential to bring large-scale benefits to society.
What is EECP?
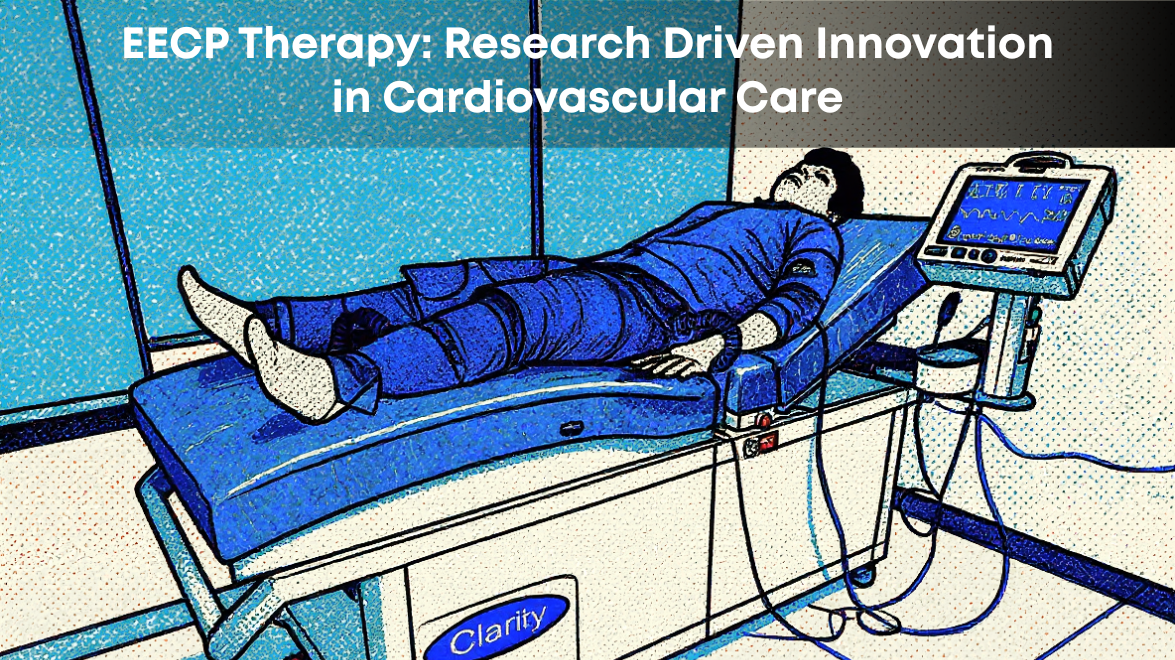
Enhanced External Counter-Pulsation (EECP) is a non-invasive outpatient therapy that enhances blood flow to the heart and other parts of the body. The procedure involves the use of cuffs wrapped around the patient’s lower limbs, which inflate and deflate in sync with the cardiac cycle—especially during diastole (when the heart is at rest). This mechanical action pushes blood toward the heart, increasing coronary perfusion pressure and improving cardiac output efficiency.
Each EECP session typically lasts one hour, and a full course includes 35 sessions over seven weeks. EECP is FDA-approved for refractory angina, and is gaining wider approval for use in heart failure, erectile dysfunction, peripheral artery disease, and stroke rehabilitation.
How Does EECP Work?
The therapeutic mechanism behind EECP is multi-faceted, involving hemodynamic, endothelial, and neurohormonal effects:
1. Increased Coronary Perfusion
The cuffs inflate sequentially from the calves to the thighs during diastole, pushing oxygen-rich blood back toward the heart. This elevates diastolic pressure and enhances coronary perfusion.
2. Reduced Cardiac Workload
By rapidly deflating just before systole, EECP reduces afterload, making it easier for the heart to pump blood, thus reducing myocardial oxygen demand.
3. Improved Endothelial Function
EECP increases shear stress on blood vessels, promoting the release of nitric oxide, a potent vasodilator, and suppressing endothelin-1 and other pro-inflammatory markers.
4. Collateral Vessel Formation (Angiogenesis)
Repeated mechanical stimulus is believed to stimulate the development of collateral arteries, enhancing long-term perfusion in ischemic tissues.

Global Research: How Much Evidence Supports EECP?
EECP is backed by multiple randomized controlled trials (RCTs), registries, and meta-analyses, particularly from the United States and Europe. Below are key studies with location, timeline, and outcomes:
1. International EECP Patient Registry (USA, 2002–2005)
This large-scale observational study tracked 1,458 patients with refractory angina undergoing EECP therapy. Results showed that 85% of patients improved by at least one Canadian Cardiovascular Society (CCS) angina class, and 70% maintained this improvement for up to two years.
Reference: Lawson WE et al., Clin Cardiol. 2005.
2. University of Florida Randomised Sham-Controlled Trial (2004–2009)
In this pioneering RCT, 42 patients with stable angina were randomised to either EECP or sham therapy. The active group showed a 51% improvement in brachial artery flow-mediated dilation (FMD) and a 30% improvement in femoral FMD, indicating robust endothelial benefits.
Reference: Casey DP, Nichols WW et al., Am J Physiol. 2011.
3. Single-Session Mechanistic Study (USA, 2009)
This trial involved 18 healthy men to observe the acute effects of a single EECP session. Brachial and femoral FMD improved significantly, suggesting that EECP may offer immediate vascular benefits, even outside of diseased populations.
Reference: Casey DP et al., J Appl Physiol. 2012.
4. MUST-EECP Multicenter RCT (USA, late 1990s)
The MUST-EECP (Multicenter Study of EECP) remains one of the most cited trials. With 139 patients across multiple U.S. centres, the study found significant increases in exercise tolerance and reduced time to ST-segment depression, supporting EECP’s anti-ischemic effects.
Reference: Arora RR et al., J Am Coll Cardiol. 1999.
5. Meta-analysis of 19 RCTs (USA & Europe, 2023)
A recent meta-analysis of 19 RCTs involving over 1,600 participants confirmed that EECP significantly improves endothelial function, particularly in patients with coronary artery disease and heart failure. The average increase in FMD was +1.96%, a clinically relevant marker of improved vascular health.
Reference: Cardiovasc Revasc Med. 2023.
Clinical Credibility and Safety Profile
EECP holds a Class IIb recommendation from the American College of Cardiology (ACC) and the American Heart Association (AHA) for the treatment of refractory angina. It is also covered by Medicare and many private insurers in the U.S., which reflects its clinical credibility and cost-effectiveness.
In terms of safety, EECP is generally well-tolerated. Minor side effects like skin irritation or muscle soreness may occur. Contraindications include severe aortic insufficiency, uncontrolled hypertension, deep vein thrombosis, or pregnancy.
Benefits to Society
The ripple effect of EECP can be significant, both in terms of individual health and public healthcare systems:
1. Alternative for High-Risk Patients
Many patients with refractory angina are not candidates for stents or bypass surgery. EECP offers a viable, safe alternative for this underserved population.
2. Reduced Hospital Admissions
Multiple studies have shown that EECP leads to fewer hospital visits and reduced use of nitrates, directly decreasing healthcare costs.
3. Quality of Life Enhancement
Patients report significant improvements in exercise capacity, mood, sleep, and energy levels—benefits that standard pharmacotherapy may not fully deliver.
4. Potential for Broader Applications
Ongoing research suggests potential benefits of EECP in:
1. Erectile dysfunction (by improving penile arterial flow)
2. Stroke rehabilitation (enhancing cerebral perfusion)
3. Diabetes (improving peripheral vascular circulation)
Challenges and Barriers
Despite its promise, EECP faces challenges:
1. Lack of widespread physician awareness
2. Limited device availability in rural or underfunded regions
3. Time commitment (35 sessions) for patients and caregivers
Conclusion
Enhanced External Counter-pulsation (EECP) stands at the intersection of biomedical innovation and evidence-based medicine. With over two decades of clinical use, validated trials from the United States and Europe, and thousands of lives improved, EECP is not just a niche therapy—it is a resilient, scalable, and underutilised solution in the global cardiovascular toolkit.
As healthcare shifts toward non-invasive, outpatient-based, and value-driven models, EECP could play a transformative role in improving outcomes and quality of life for millions, while easing the burden on overtaxed healthcare systems.